Updated Friday, December 5, 2025
The New York Academy of Medicine reaffirms our commitment to vaccine science and evidence-based guidelines that are the cornerstones of public health progress. We stand in opposition to the decision today by the Centers for Disease Control and Prevention’s (CDC) Advisory Committee on Immunization Practices (ACIP) to narrow the agency’s hepatitis B immunization guidance for newborns.
The Science is Clear
Vaccines are one of medicine’s greatest advances, with decades of strong, validated evidence supporting immunization. In the United States over the past 30 years, childhood vaccinations have prevented an estimated 508 million illnesses, 32 million hospitalizations, and over one million deaths.[1] The return on investment from childhood vaccinations is $11 and for adult vaccination up to $19 for every dollar spent, not only saving lives but preserving a healthier workforce and our national economy.[2]
These outcomes reflect the dedication of researchers and healthcare providers working to keep communities safe.
Stance from Other Leading Scientific and Medical Organizations
Our position aligns with organizations such as the American Medical Association[3] and the American Academy of Pediatrics[4], who today reaffirmed it would continue to recommend the hepatitis vaccine for all newborns. Leading scientific and medical organizations collectively affirm that vaccines undergo thorough clinical trials and safety monitoring, meeting high standards of scientific rigor, and recognize that immunizations save lives and protect public health by preventing severe disease and hospitalizations. We stand with the Northeast Public Health Collaborative in advancing science-driven strategies to strengthen vaccine confidence and protect the health of every community.[5] Further, according to Acting Commissioner of the New York City Department of Health and Mental Hygiene Dr. Michelle Morse: “The New York City Health Department strongly recommends maintaining the current vaccination schedule, beginning with the birth dose, to continue to protect our youngest New Yorkers from preventable illnesses. Delaying this effective vaccine puts infants at risk.”[6]
Building Trust
Trust in vaccines depends on ongoing transparency and scientific credibility. Through research, education, and community partnerships, we are committed to providing accurate, evidence-based information.
The following resources may be helpful to individuals seeking trustworthy information on vaccine practices:
- National Foundation for Infectious Diseases
- NMA Statement on ACIP Vote to Roll Back Universal Hepatitis B – National Medical Association
- New York City Department of Health and Mental Hygiene Letter to Providers (Dated December 5, 2025)
- Northeast Public Health Collaborative – NYC Health
- Securing the Foundation: Stakeholder Insights and Strategies for Maintaining a Strong Vaccine Infrastructure Across the US
For parents who want to stay updated on requirements for New York schools, these resources are available:
- School Immunization Requirements (New York State Department of Health)
- Immunizations (New York City Public Schools)
[1] Zhou F, Jatlaoui TC, Leidner AJ, et al. Health and Economic Benefits of Routine Childhood Immunizations in the Era of the Vaccines for Children Program — United States, 1994–2023. MMWR Morb Mortal Wkly Rep 2024;73:682–685. DOI: http://dx.doi.org/10.15585/mmwr.mm7331a2
[2] El Banhawi H., Chowdhury S., Neri M., Radu P., Besley S., Bell E., Brassel S., Steuten L., , Socio-Economic Value of Adult Immunisation Programmes (2024). Contract Research. Available from https://www.ohe.org/publications/the-socio-economic-value-of-adult-immunisation-programmes/.
[3] An open letter to the American public on respiratory virus vaccines | American Medical Association
[4] Vaccination Recommendations by the AAP
[5] Hepatitis B Immunization is Critical to Protect All Newborns, American Academy of Pediatrics
[6] New York City Reiterates Importance of Hepatitis B Birth Dose for All Newborns – NYC Health
Including a Discourse with Notable Media on Combating Misinformation
New York, NY (November 28, 2025) – The 178th Anniversary Discourse, Annual Awards and Meeting of the Fellows at New York Academy of Medicine takes place on Monday, December 1 at 5:30 p.m. The gathering will celebrate health science leadership in 2025 and induct a record new class of fellows and members at the New York Academy of Medicine building located at 1216 Fifth Avenue at 103rd Street. Among the evening’s highlights, a dialogue among leading journalists about how to communicate health science advances in a time of polarization, and leading health scientists will be celebrated:
- Five individuals, including Regina Benjamin, MD, MBA, the 18th U.S. Surgeon General; Jennifer Doudna, PhD, Nobel laureate in chemistry; Peter Jay Hotez, MD, PhD, Dean for the National School of Tropical Medicine at the Baylor College of Medicine; Timothy R. B. Johnson, MD, Bates Professor of the Diseases of Women and Children and Chair of Obstetrics and Gynecology, University of Michigan; Mary Woolley, president and CEO of Research!America; and the Rockefeller Foundation and the Carnegie Corporation will be awarded for their health impact
- The induction of 131 New York Academy of Medicine fellows and members
- A roundtable panel discussion about the ongoing dangers of health misinformation
“We are delighted to welcome people across our communities, from accomplished health scientists and leaders, new fellows from hundreds of organizations throughout the tristate area, and a stimulating discourse panel of distinguished journalists to our annual meeting,” Ann Kurth, PhD, CNM, MPH, president of New York Academy of Medicine said. “We are gratified to expand the base of accomplished fellows and members, especially this year when standing for public health is so crucial for all of us who want better health for our families and communities. We look forward to working with them to help realize New York Academy of Medicine’s mission of healthier, longer lives for all.”
The roundtable discussion follows the evening’s theme: promoting health by combating health misinformation. Three prominent New York journalists (Dhruv Khullar, MD, of The New Yorker, Brian Lehrer of WNYC, and Apoorva Mandivalli of The New York Times) will discuss this theme at length while drawing from their experiences. Harriet Washington, renowned author and fellow at New York Academy of Medicine, will moderate the conversation. Wayne J. Riley, MD, MPH, MBA, MACP, chair of the board of trustees at New York Academy of Medicine, expressed enthusiasm about the roundtable.
“Health misinformation is something we can’t ignore, and I don’t think our communities should, either,” Dr. Riley said. “Communicating accessible, trustworthy, and accurate health information is paramount for everyone from practitioners to patients. We do a disservice to ourselves and others if we do not stand up for and promote best-evidence health solutions.”
Health progress is only made possible through scientific advances informed by community buy-in and engagement. New York Academy of Medicine is grateful to all who are attending the 2025 annual awards and meeting of the fellows. Together, we can help enable healthier, longer lives for everyone.
When New York Academy of Medicine was founded, fossil fuel pollution that would come to heat the earth was very low; now, nearly two centuries of dramatically higher ‘greenhouse gas emissions’ (see graph) has led to warming that affects the health of humans and all other species that are entwined with our survival and wellbeing.
Last week, the 30th annual United Nations Climate Change conference (COP 30) took place in Belem, Brazil, with tens of thousands gathered for global discourse about how to collectively combat this crisis. In the same week, the United States (which did not attend COP for the first time ever) proposed to dismantle protections for the clean air that we all want to breathe, and for endangered species.

Scientific Consensus: Humans Contribute to a Warming Planet that Harms our Health Outcomes
The scientific community has been sounding the alarm and dangers of our warming planet for decades. The National Oceanic and Atmospheric Administration (NOAA) noted that 2024 was the hottest year in recorded history. The documented impact on human health includes:
- 8 million people die prematurely every year due to fossil fuel-born air pollution
- Heat-induced deaths among people over 65 have significantly increased since 2010
- Billion+ dollar climate disasters are happening more often; in 2024 alone, there were 27 events costing US taxpayers and employers $182.7 billion
The consensus is clear, from research scientists and intergovernmental bodies to US citizens themselves, 63% of whom said in 2024 they are worried about ‘cimate change.’ Climate impact on human health is accelerating, but it’s important to note that there are actions to take, and that health professionals can be trusted sources to help protect patients, communities, and health systems.
COP 30: (Most) Nations United for Climate Action
Almost 200 countries attended COP 30, mirroring the 195 nations signed the groundbreaking Paris Climate Accords in 2015, which set the goal of holding average global temperature to well below 3.6 degrees Fahrenheit (2 degrees Celsius) above pre-industrial levels. A 2024 survey of hundreds of leading Intergovernmental Panel on Climate Change (IPCC) scientists showed, however, that almost half anticipate at least 3°C of warming.
COP 30 covered dozens of meetings each day, many of them discussing health impacts: from adapting the health sector to climate change, pivoting finance towards health needs for sustainable development, and regenerative agriculture for healthier diets. During COP 30, the Brazilian government launched the Belem Health Action Plan to help the country’s health sector adapt to the rigors of the climate crisis. New York Academy of Medicine participated in the development of this plan through the World Health Organization’s (WHO) Alliance for Transformative Action on Climate and Health (ATACH).
The U.S.: The Elephant Not in the Room but Trampling the Grass…
While the U.S. delegation was absent from COP 30 in Belem, back in Washington, D.C., the Trump administration proposed to gut the Clean Water and the Endangered Species Acts. “We were disappointed to see that the federal government did not send an envoy to COP 30. We were more disappointed to see the proposed destruction of longstanding, consensus government guidance that helps keep our water safe to drink and that supports other species who might help us discover the next cure for disease.” Ann Kurth, PhD, CNM, MPH, president of New York Academy of Medicine said. “A warming planet is hurting human health and addressing it takes the public and private sectors working in tandem at all levels.”
While the executive branch didn’t send delegates to COP 30, dozens of U.S. government officials at various levels of government did attend on behalf of their communities. From governors like Gavin Newsome of California to mayors like Katrina Evans of Campti, Louisiana, it was encouraging to see government officials from large states to small towns attend to address a cause that affects Americans across any political divides.

Resources to Fight Climate Change Locally
A hotter planet is a global problem, but the globe is comprised of communities. You and your colleagues can work on these issues at the local level, including with patients and in our hospitals. We can educate ourselves about emergency preparedness for extreme storms, flooding, and heat waves. It is important to keep in mind that:
- Climate change impact is now
- Effects on human health are growing
- We can act
- Health professionals are key for action
Here is a non-exhaustive list of trustworthy resources:
- Green your building (Clean Energy hubs)
- New York Academy of Medicine’s Heat Vulnerability Index Maps
- New York State Department of Health’s Air Quality Index
- New York State Department of Health’s Cooling Centers
- The U.S. Centers for Disease Control and Prevention’s (CDC) Environmental Public Health Tracker
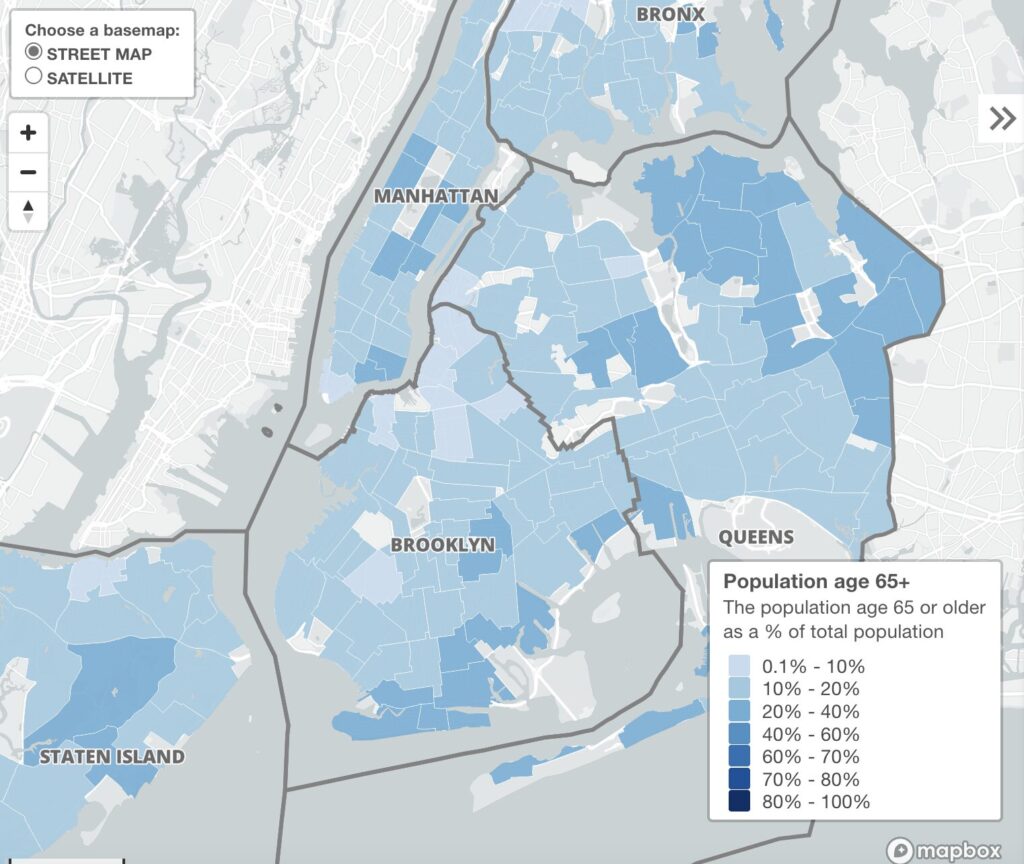
Snapshot of New York Academy of Medicine’s Heat Vulnerability Index Map
“Fighting climate risk starts at the local level. I’m proud of the work that we have done with the Heat Vulnerability Index Maps,” said Kathryn T. Hall, PhD, MPH, senior vice president, research at New York Academy of Medicine. “The map can be used by anyone who accesses it online. Each of the categories—climate, demographics, housing, public safety, socioeconomics, and voters—have detail like employment status, race/ethnicity, and health insurance type, to assess where people need support.”
Our planet is warming; magnified by human activity; the evidence is overwhelming and felt by most of us, no matter what it is called. As the effects grow ever more apparent, we remain steadfast in keeping our community informed about how to advocate for a more protected planet in which we can all live healthier, longer lives.
You can comment on proposed changes to the Clean Water/Endangered Species Act until December 20. There are four dockets available for public comments:
- Endangered and Threatened Wildlife and Plants; Listing Endangered and Threatened Species and Designating Critical Habitat
- Endangered and Threatened Wildlife and Plants; Interagency Cooperation Regulations
- Endangered and Threatened Wildlife and Plants; Regulations Pertaining to Endangered and Threatened Wildlife and Plants
- Endangered and Threatened Wildlife and Plants; Regulations for Designating Critical Habitat
Healthcare Is a Shared Mission: Imperative to Support All Health Professionals
Healthcare is, by its very nature, collaborative. Health professionals – including nurses, physicians, public health professionals, and many others – stand together to support patients and populations. Achieving a vision where everyone has what they need for healthier, longer lives depends on a health workforce that is both diverse and fully integrated. Yet a proposed ruling from the U.S. Department of Education threatens this model by reclassifying essential health science degrees (including nursing, public health, physician assistant studies, audiology, social work, and physical therapy) and stripping them of their “professional” status.
A Crisis by the Numbers
This proposal fails to acknowledge the current deep vulnerabilities across the healthcare ecosystem, where workforce gaps that affect nursing, public health practitioners, and clinical specialists are widening. Imposing new barriers, such as those recommended by the Department of Education, risks destabilizing the already stressed health system.
Nearly half of the nation’s public health workforce left their positions during the COVID-19 pandemici. Experts warn that without significant investment in education, New York will face persistent shortages in public health professionals through the next decadeii.
The nursing shortage remains especially acute: tens of thousands of positions nationwide remain vacant, and workforce projections indicate persistent shortages for years to come. Meanwhile, data from the American Association of Colleges of Nursing show that more than 80,000 qualified applicants were turned away from U.S. nursing schools in 2022 due to limited faculty and resourcesiii, which indicates a pressing shortage of advanced practice nurses and nursing faculty (without whom workforce expansion is impossible).
Notably, in New York Academy of Medicine’s 2025 Fellows cohort, 47% are nurses: an impressive figure that nonetheless belies a discrepancy with workforce need.
The Threat to Everyone’s Health is Profound
The Department of Education’s proposed reclassification arises from Public Law 119–21 (signed 7/4/2025), which seeks to redefine eligibility for federal financial aid by limiting what is considered a “professional” degree. Under this new definition, students in programs no longer deemed “professional” would be ineligible for the Graduate PLUS Loan program, a funding source essential for many seeking advanced degrees in health science professions.
Should this be enacted, countless students in nursing, public health and other critical health disciplines could lose access to crucial financial support. The scope of this proposed restriction is extensive, including nursing, public health, physician assistant studies, audiology, social work, and physical therapy.
Restricting financial aid in this manner is likely to:
- Limit entry to these fields, particularly for students from economically disadvantaged backgrounds.
If this happens, we will reverse progress toward a workforce that reflects the diversity of our communities and that serves health needs from prevention to primary to specialty care.
- Undermine the recognition and support of critical health professions.
Eroding the status of these degrees would diminish respect for professionals and weaken confidence in the broader health system, at a time when public trust and evidence-based leadership are especially vital.
As New York Academy of Medicine President Ann Kurth has emphasized: “When one part of the health team is undermined, care for all is compromised. Every role, from bedside nurses and public health workers to scientists and policy leaders, must be supported and empowered in order to build healthier communities.”
Response from Other Leading Organizations
Leading organizations across the health sector share these concerns.
The American Nurses Association has cautioned that restricting federal aid will intensify shortages and undermine equity in nursing education.iv
The Association of Schools and Programs of Public Health has warned that excluding public health degrees from “professional” status is short-sighted and dangerous, undermining the nation’s ability to prepare practitioners who protect population health.v
The Council on Social Work Education has warned that redefining professional degrees will limit access to social work education and weaken the pipeline of mental health providers.vi
Policymakers should engage these stakeholders to ensure that financing mechanisms match the rigor and value of these programs.
A Call to Action
This issue is a broad health emergency for all health professionals and all of us who rely on them, with implications for every facet of prevention and care delivery.
New York Academy of Medicine is committed to working in concert with our diverse community of Fellows, which includes nurses and other clinicians, researchers, educators, and public health leaders, to oppose this measure.
We call on the Department of Education to recognize that the nation’s health depends on a fully supported, interdisciplinary workforce. The Department is expected to release a Notice of Proposed Rulemaking in the coming weeks, opening a public comment period in which New York Academy of Medicine will participate.
It is imperative for health professionals and consumers to unite in ensuring that all members of the health workforce are recognized as essential, rigorous, and invaluable.
i Hare Bork R, Robins M, Schaffer K, Leider JP, Castrucci BC. Workplace Perceptions and Experiences Related to COVID-19 Response Efforts Among Public Health Workers — Public Health Workforce Interests and Needs Survey, United States, September 2021–January 2022. MMWR Morb Mortal Wkly Rep. 2022;71(29):920–924. doi:10.15585/mmwr.mm7129a3
ii Center for Health Workforce Studies. (2023). The Health Care Workforce in New York State: Trends in the Supply of and Demand for Health Care Workers. Rensselaer, NY: School of Public Health, University at Albany, State University of New York.
iii American Association of Colleges of Nursing. (2023). 2022-2023 Enrollment and Graduations in Baccalaureate and Graduate Programs in Nursing. Washington, DC: AACN.
iv American Nurses Association. Statement on Federal Student Loan Policy and Nursing Education.
v Association of Schools and Programs of Public Health. Exclusion of Public Health Degrees from Professional Status.
vi Council on Social Work Education. Statement on DOE Definition Limiting Access to Social Work Education.
We largely know what makes people healthy, and what doesn’t. Access to nutritious food is one key driver of health. So, it is doubly unjustifiable to threaten food that children, older people, and families need to thrive and contribute to the economy and to communities. Stopping coverage of the Supplemental Nutrition Assistance Program (SNAP) is unfair and unwise. New York Academy of Medicine calls for the US government to meet its obligation to run the SNAP program as Congress has designated. At New York Academy of Medicine we have always supported the best practices to protect and advance health for all, from advocating for vaccines, to guiding communities through the COVID pandemic, to today, supporting the reinstalment of SNAP benefits for all recipients.
Basic Nutrition is a Prerequisite for Health
The ongoing federal government shutdown is already affecting communities across the nation and here in the tri-state area. This past Friday, two federal judges determined that the federal Supplemental Nutrition Assistance Program (SNAP) should remain in place during the ongoing government dispute. However, the Trump administration recently stated they would stated they would not supply any SNAP benefits until the government shutdown has concluded. This is concerning from a health perspective to our communities because 1.8 million New Yorkers are vulnerable to food scarcity and malnutrition. At New York Academy of Medicine, we are aware that the brunt of this impact is happening to members of our communities who are least able to cover this crucial gap.
“We have always known how crucial nutrition is to personal and civic health,” Ann Kurth, PhD, CNM, MPH, New York Academy of Medicine’s president said. “We have 10,000 cookbooks and related items in our medical historical library that show how people have used food as literal medicine for as long as societies have existed. Adequate food for pregnant people, growing children, people with disabilities, older folks, and everyone in between, benefits us all.”
Stances from Other Leading Health Advocacy and Food Security Organizations
Our position aligns with other organizations whose expertise led them to the conclusion that this suspension of SNAP benefits needlessly harms the most resource-scarce New Yorkers. We agree with Food Bank for NYC that New Yorkers should stand together to combat hunger and malnutrition as the government shutdown continues. New York Health Foundation rightly states that no one should have to decide between eating, keeping the lights on, or paying rent. We stand shoulder-to-shoulder with WIN (formerly Women in Need) in recognizing that SNAP benefits are essential to covering baby formula and children’s meals for thousands of families across the five boroughs.
Our Commitment
New York Academy of Medicine remains committed to food security and access to nutritious foods for all by:
- Advancing equitable access to a nutritious diet: everyone needs food
- Supporting rigorous, independent food security and nutrition research
- Promoting clear communication about the link between access to nutritious food and positive health outcomes
- Fostering dialogue and action between communities and providers
Building Trust
Access to nutritious food is a fundamental baseline for healthy people and healthier communities. Through research, education, and community partnerships, we are committed to providing accurate, evidence-based information.
If you, your family, or anyone else you know relies on SNAP benefits, here are some resources you might find helpful:
- The Legal Aid Society: What You Need to Know About Cash Assistance & SNAP From the NYC Human Resources Administration (HRA)
- Mutual Aid Society: A comprehensive list of NYC-based food assistance programs and nonprofits
- City Harvest: Food being distributed freely via their interactive Food Map
- Food Bank for NYC: Find a Food Pantry Near Me
- Hunger Free America: SNAP Benefits Access
New York Academy of Medicine is determined to help all New Yorkers and members of our wider community live healthier, longer lives. To that end, we will continue to keep you informed about the ongoing situation with SNAP benefits and other food security issues.
 |
 |
| Ann Kurth, PhD, CNM, MPH President, New York Academy of Medicine |
Wayne J. Riley, MD, MPH, MBA, MACP Chair, Board of Trustees New York Academy of Medicine |
New York, NY (October 23, 2025) – New York Academy of Medicine hosted its 30th annual gala on Tuesday, October 21, 2025. Nearly 250 people in attendance gathered in the organization’s historic library to honor three healthcare champions and to unite behind one unified purpose: healthier, longer lives for all.
Kristine Johnson, an Emmy-award winning CBS News New York anchor and TV news journalist, hosted the gala for the first time. Johnson welcomed all in attendance with her signature conversational style, charm, and warmth.
“Your presence here tonight is a testament to your compassion and your commitment to our shared mission,” Johnson said during her opening remarks. “Tonight, we stand together, united by a shared goal of healthier, longer lives for everyone. It’s not just an aspiration; it’s a responsibility we all embrace together.”
Johnson welcomed Ann Kurth, PhD, CNM, MPH, New York Academy of Medicine president, who spoke passionately about the nonprofit’s mission and exciting work on the horizon. Dr. Kurth emphasized that New York Academy of Medicine is both a long-standing and forward-looking institution.
“From pioneering public health and sanitation, from transforming safer childbirth, and accessible vaccine programs, to tackling the urgent challenges of a warming climate, we have consistently stood at the forefront of progress,” she explained. “By keeping our eyes on the future, we turn the possibility of healthier, longer lives into a reality for our fellow New Yorkers and for communities around the globe.”
Each of New York Academy of Medicine’s three annual awards were given to deserving health equity advocates at the annual gala. The first award, the Healthcare Legacy award, was given to John ‘Jack’ W. Rowe, MD, Julius B. Richmond Professor of Health Policy and Aging, Columbia University Mailman School of Public Health. Johnson asked Dr. Rowe to talk in depth about the term ‘successful aging’ that he coined in 1987. He is a subject matter expert regarding addressing health outcomes in older adults.
“At any given age, say 65, with advances in the prevention of disease and in treatment, the portion of remaining life going forward would be more healthy and less disabled. That’s the optimistic vision,” he elaborated before providing important nuance. “We now have emerging evidence that it’s only happening for people in higher socioeconomic groups.”
The Bold and Brave award was given next to Tom Wright, president and CEO of Regional Plan Association (RPA), in recognition for his innovative urban planning work and advocacy. Wright spoke about some of the challenges and opportunities in creating more livable cities for all, and the effect that urban planning has on health outcomes. He talked about the potential successes of congestion pricing, including health outcomes.
“Traffic fatalities in New York City are down by about a third this year,” Wright emphasized, referencing data on the first six months of this year compared to the previous one, and noting that air quality comparisons will be another measure to watch.
The evening’s final honor, the Health Equity Champion Award, was given to Pat Wang, president and CEO of Healthfirst, who has worked tirelessly in support of high-quality, equitable care. Wang spoke about the pressing need to focus on providing dignified care for vulnerable populations.
“We all are driven by personal experience, and health is personal,” she explained. “When you start from that premise of doing a good thing for communities and people who are uninsured, the question is ‘What’s next? What do we do to make sure that people have the experience and the care they want?’”
Each awardee shared a unique message and perspective, yet all emphatically spoke in alignment with New York Academy of Medicine’s mission to create healthier, longer lives for all. The Academy is grateful to Kristine Johnson for being a gracious emcee, to our three honorees for sharing their knowledge and advice, and for all in attendance for their time, generosity, and for building a forward-looking health advocacy community alongside us.
About New York Academy of Medicine
New York Academy of Medicine (NYAM) is a leading voice for innovation in population health. With over 178 years of history, NYAM is committed to a future where everyone has what they need for a healthier, longer life. Guided by the expertise of its 1,800 Fellows, a world-class historical medical library, and its convening, capacity-building and community-informed research, NYAM creates actionable solutions to today’s most pressing health challenges. To learn more, visit www.nyam.org.
Media Contact:
Max Mallet
Marketing Content Manager
[email protected]
212-822-7314
New York, NY (October 17, 2025) — New York Academy of Medicine is proud to announce its upcoming 30th annual gala to celebrate health luminaries and to empower healthier, longer lives for all. The gala will take place on Tuesday, October 21, 2025, from 6:00-9:00 P.M., at the Academy’s home on Museum Mile.
“This year’s gala is significant for many reasons, among them being the celebration of the 100th anniversary of New York Academy of Medicine opening the doors of our beautiful building on Fifth Avenue,” President Ann Kurth, PhD, CNM, MPH, said. “We are excited and proud to bring our community together in our historical library to honor three exemplary leaders, innovators, and friends of New York Academy of Medicine.”
This year’s honorees are:
- John ‘Jack’ W. Rowe, MD, Julius B. Richmond Professor of Health Policy and Aging, Columbia University Mailman School of Public Health, will be honored with this year’s Healthcare Legacy award. Dr. Rowe is a pioneering researcher whose knowledge of health systems and the healthcare industry has benefited New Yorkers and older adults nationwide.
- Tom Wright, president and CEO of Regional Plan Association (RPA), will be bestowed with this year’s Bold and Brave Award. Wright has passionately worked to address climate change and advocated for affordable, livable communities in the greater New York City region.
- Pat Wang, president and CEO of Healthfirst, will receive this year’s Health Equity Champion Award. Wang has demonstrated proactive leadership and unwavering support towards quality and equitable care for all. She has emphasized focusing on those who experience healthcare disparities.
This year, New York Academy of Medicine will welcome a new emcee, Kristine Johnson, anchor and TV news journalist for CBS News New York.
“New York Academy of Medicine is grateful to have Kristine Johnson, a multi-Emmy award-winning journalist, lend her talents to our annual gala,” Dr. Kurth elaborated. “She’s a familiar face and voice that New Yorkers trust. With her enthusiasm and insightfulness, she will bring so much life to our program. We are thrilled to welcome her to the Academy for the first time.”
Click here to learn more about this year’s annual gala. Thank you for your generous support that helps us empower healthier, longer lives, for all.
About New York Academy of Medicine
New York Academy of Medicine (NYAM) is a leading voice for innovation in population health. With over 178 years of history, NYAM is committed to a future that where everyone has what they need for a healthier, longer life. Guided by the expertise of its 1,800 Fellows, a world-class historical medical library, and its renowned research efforts, NYAM creates actionable solutions to today’s most pressing health challenges. To learn more, visit www.nyam.org.
Media Contact:
Max Mallet
Marketing Content Manager
[email protected]
212-822-7314
New York, NY – August 7, 2025 – New York Academy of Medicine (NYAM) has officially released its 2024 Annual Report, showcasing a year of innovation, groundbreaking research, and steadfast commitment to advancing population health. The report reflects NYAM’s dedication to creating healthier, longer lives for all through impactful engagement and forward-thinking solutions.
For 178 years, New York Academy of Medicine has stood as a leader in health progress, consistently addressing society’s most pressing health challenges. The 2024 Annual Report highlights the organization’s work across New York City and beyond, including initiatives focused on improving health outcomes, addressing disparities in care, and tackling issues such as mental health, maternal and child health, and climate resilience.
“Although the world around us may feel unpredictable, New York Academy of Medicine remains focused,” said Ann Kurth, PhD, CNM, MPH, President of NYAM. “We passionately protect evidence-based knowledge, advance the next generation of leaders, and work to build trust in health and medicine.”
This year’s achievements include:
- Innovative research efforts aimed at extending both lifespan and healthspan.
- Inclusive convenings of policymakers, health professionals, and community voices to address urgent health topics.
- A newly inducted, diverse class of Fellows and editorial leadership at the Journal of Urban Health.
The report also underscores New York Academy of Medicine’s emphasis on partnerships. Despite declining federal funding to public health programs, NYAM’s voice continues to create meaningful pathways to effective solutions.
“We are deeply connected to the communities we serve,” Kurth added. “This means we are able to see what is happening on the ground, evaluate the impact of interventions, amplify community voices, and convene leaders to drive action.”
To explore these initiatives, examine the data, and learn more about NYAM’s ongoing efforts, read the full 2024 Annual Report at NYAM 2024 Annual Report – NYAM Annual Report.
About The New York Academy of Medicine
New York Academy of Medicine (NYAM) is a leading voice for innovation in population health. With over 178 years of history, NYAM is committed to advancing healthier, longer lives for all. Guided by the expertise of its 1,800 Fellows, a world-class historical medical library, and its renowned research efforts, NYAM creates actionable solutions to today’s most pressing health challenges. To learn more, visit www.nyam.org.
Media Contact:
Jennifer Russo
Director of Marketing
[email protected]
212-822-7304
NEW YORK, NY (July 30, 2025) — New York Academy of Medicine (NYAM) has appointed three nationally recognized health leaders to its Board of Trustees, reinforcing its commitment to healthier, longer lives for everyone: Debra Albert, DNP, MBA, RN, NEA-BC; Lorna Friedman, MD, MBA; and Jen Radin, MBA, MPH.
“NYAM is thrilled to welcome these innovative health leaders to our Board of Trustees,” said Ann Kurth, PhD, CNM, MPH, President of New York Academy of Medicine. “Their diverse expertise and unwavering commitment to health equity will accelerate our mission and deepen our impact across communities.”
The addition of these new trustees underscores NYAM’s bold vision: a world where everyone has what they need to live healthier, longer lives. With decades of leadership in nursing, global health strategy, and health innovation, this new cohort will help steer NYAM’s future-facing initiatives.
“I extend a heartfelt welcome to our newest Trustees, whose dedication, wisdom, and passion will strengthen our work at this critical moment in public health,” said Wayne J. Riley, MD, MPH, MBA, MACP, NYAM Board Chair and President of SUNY Downstate Health Sciences University.
“I am honored to join the Board of New York Academy of Medicine and the incredible group of Trustees who are collaborating to support the mission of extending healthspan for all populations in New York City by focusing on healthy births, greater longevity for aging adults, and urban strategies for living on a warming planet,” said Jen Radin, MPH, MBA. “It’s truly an honor to be counted among such a committed and deeply experienced group of health ecosystem business leaders.”
“I am honored to serve on the Board of Trustees for New York Academy of Medicine,” added Debra Albert, DNP, MBA, RN, NEA-BC. “Working with this distinguished group of healthcare leaders to achieve the vision of ensuring that all people have access to quality care to live healthier lives has never been more important. I look forward to the work ahead to make this a reality for our communities.”
These new Trustees bring a wealth of experience across clinical care, health strategy, and innovation:
Debra Albert, DNP, MBA, RN, NEA-BC is Chief Nursing Officer and Senior Vice President of Patient Care Services and the Lerner Director of Health Promotion at NYU Langone Health. Dr. Albert is responsible for ensuring contemporary, evidence-based nursing practice across all of NYU Langone Health’s care settings. She is a recognized leader in patient safety, transformative systems leadership, staff development and formal succession planning. She leads a diverse team of nursing leaders focused on interdisciplinary collaboration to achieve optimal patient outcomes. As a mentor for nursing and female leaders, she develops programs that help build sustainable workforces. In addition, Dr. Albert is on the strategic steering committee of the Vizient/AACN Nurse Residency Program, the Rush DNP Advisory Council and the Walden University Board of Directors.
Lorna Friedman is Senior Partner of Health Transformation and Sustainability at Mercer Marsh Benefits. Dr. Friedman has extensive experience designing health solutions for multinational employee populations including risk analysis, operational and benefit design, onsite and digital delivery. Previous roles include Partner in Mercer’s Global Health Management practice, working with organizations on their health strategies. Dr. Friedman trained in Pediatrics at The Children’s Hospital of Philadelphia. She has held academic and teaching positions at University of Pennsylvania and Cornell Medical College and holds an MBA from Columbia University. She has served on several boards with a focus on improving access to health including the Global Business Group on Health, The American Council on Exercise and the March of Dimes. Dr. Friedman was the recipient of the Nancy C Barnhart award for Child Advocacy and is a member of the YWCA Women’s Leadership Academy.
Jen Radin is Life Science and Healthcare Principal at Deloitte. Ms. Radin brings more than 25 years of life sciences and health care industry experience partnering with life sciences and health care system executives to embrace transformation, helping them leverage data, next-gen technologies, and the health ecosystem through applied innovation to design new models of clinical care and future-proof their business. She is deeply committed to navigating the rapidly changing health ecosystem and creating value on the journey to health and wellness. Ms. Radin is a principal in Deloitte & Touche LLP and is a nationally acclaimed speaker on the topics of Future of Health and Future of Work as well as the women’s health marketplace. Ms. Radin focuses on helping clients so they can unlock opportunities in the women’s health market and has been instrumental in helping advance the mission of the Deloitte Health Institute. She also oversees strategic efforts to help ensure that optimal health outcomes are considered across the organization, in its services and offerings, and in interactions with clients and the community.
She is the co-founder and executive sponsor of Deloitte’s Physician Leadership Academy, which supports the evolving leadership capabilities of clinician leaders in the era of clinical health care.
About New York Academy of Medicine
New York Academy of Medicine (NYAM) is a leading voice for innovation in population health. Building on its 178-year legacy, NYAM continues to drive forward-thinking solutions to today’s most pressing health challenges: from aging populations to climate resilience. Through our innovative research, 1,800 esteemed Fellows, a world-class historical library, and an unparalleled power of convening, we create real-world advances for population health.
New York, NY, Feb 21, 2025 (GLOBE NEWSWIRE) — THE NEW YORK ACADEMY OF MEDICINE AWARDS TWO 2025-2027 JEREMIAH A. BARONDESS FELLOWSHIPS IN THE CLINICAL TRANSACTION
Dr. Jessica Lichter is an Assistant Professor and academic hospitalist at Elmhurst Hospital, part of the New York City Health + Hospital public health system located in the Borough of Queens, an affiliate of the Icahn School of Medicine at Mount Sinai
Dr. Shyam Sundaresh is an Assistant Professor of Medicine at the Icahn School of Medicine at Mount Sinai.
The New York Academy of Medicine (NYAM), in collaboration with the Accreditation Council for Graduate Medical Education (ACGME), is pleased to announce that the 2025-2027 Jeremiah A. Barondess Fellowship in the Clinical Transaction is awarded to Dr. Jessica Lichter and Dr. Shyam Sundaresh.
Jessica Lichter, MD, is a hospitalist at Elmhurst Hospital, NYC Health + Hospitals, (Mount Sinai Affiliate), who plans to further develop and evaluate an innovative simulation platform that she developed, ChatMD, to improve communication skills related to code status discussions in the hospital setting and to enhance humanistic care among internal medicine residents.
Shyam Sundaresh, MD, is an Assistant Professor in the Division of General Internal Medicine, Mount Sinai Hospital who plans to implement, evaluate, and disseminate the use of Brief Direct Observation of clinical encounters to provide feedback to internal medicine residents on their communication skills for patients with mental health conditions, including depression and anxiety, in the ambulatory care, general internal medicine setting.
The ACGME and NYAM will recognize Drs. Lichter and Sundaresh at the ACGME Annual Educational Conference, to be held in Nashville, Tennessee from February 20th to 22nd.
The Barondess Fellowship is awarded to junior faculty members in internal medicine to enhance medical students’ and residents’ training in the clinical transaction, a fundamental element of clinical care. The two-year, $50,000 fellowship aims to improve the patient experience by innovating and strengthening the critical skills that characterize the clinical transaction, including communicating with patients, conducting the physical exam, and applying clinical reasoning.
“Preparing clinicians to enhance their communication skills, a crucial element of the clinical partnership between providers and patients could not be more critical toward advancing better health for all,” said NYAM President Ann Kurth, PhD, CNM, MPH.
“Effective communication is a critical element of patient care. It builds trust and strengthens the bond between patient and physician. The ACGME is delighted to recognize Drs. Lichter and Sundaresh, and we look forward to the outcomes of their projects,” said ACGME President and CEO Debra Weinstein, MD.
-More-
“My current research focuses on harnessing artificial intelligence (AI) to enhance physicians’ communication skills, particularly around end-of-life care. I am deeply honored to receive the Barondess Fellowship to pursue this work, and view it as both an opportunity and responsibility to create an AI that strengthens our humanity as physicians rather than diminishes it,” said Dr. Jessica Lichter.
Dr. Lichter is an assistant professor and an academic hospitalist at Elmhurst Hospital, an affiliate of the Icahn School of Medicine at Mount Sinai. She is a trained simulation specialist and completed a fellowship in medical simulation at the NYC Health + Hospitals Simulation Center. She completed residency in internal medicine at New York University and medical school at Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia. Prior to her medical career, Dr. Lichter obtained a master’s degree in neuroscience from the University of California, San Diego and a bachelor’s degree from Duke University. Her current research focuses on using conversational artificial intelligence to enhance communication skills among clinicians.
“We face a growing shortage of mental health care. Even more concerning, is that many who need mental health care the most are disproportionately affected by this shortage. By training Internal Medicine residents in mental health care, we can help bridge this gap. I am incredibly grateful to NYAM and the ACGME for awarding me the Barondess Fellowship, providing an opportunity to address this critical educational need,” said Shyam Sundaresh, MD.
Dr. Sundaresh is currently an Assistant Professor at the Mount Sinai Internal Medicine Residency Program. He graduated medical school at the Case Western Reserve University School of Medicine, and trained at an Internal Medicine Primary Care Residency at Weill Cornell Medical Center. Before a career in medicine, Dr. Sundaresh completed a Bachelor of Arts in Music at Northwestern University. He then became a music teacher for people with special needs. This work inspired his eventual focus in communication skills and mental health within primary care.
Dr. Jessica Lichter
The 2025-2027 Recipient of the Jeremiah A. Barondess Fellowship in the Clinical Transaction

Dr. Shyam Sundaresh
The 2025-2027 Recipient of the Jeremiah A. Barondess Fellowship in the Clinical Transaction
